Dunsborough Physiotherapy Centre SPRIG program (Stretch Proactively to Reduce Injury to Growth-plates)
 SPRIG Injury Prevention Program
SPRIG Injury Prevention Program
Dunsborough Physiotherapy Centre has recently released an injury prevention program aimed at reducing growth-plate injury rates in children and adolescents in Dunsborough and surrounding areas: the SPRIG program. This program has been created by Ben Liston: a Dunsborough physio with over 20 years of experience. Three common growth-plate injuries are addressed by the program: Osgood Schlatter disease, Sinding-Larsen-Johansson syndrome and Sever's disease. The program focusses on inflexibility of muscles groups related to growth-plate injuries. At present Dunsborough Physiotherapy Centre is targeting junior football, soccer, netball, and basketball players: supplying information to the associated junior sports committees, coaches and parents in relation to appropriate stretching methods to help reduce growth-plate injury incidence.
At Dunsborough Physiotherapy Centre we are committed to reducing injury rates in children / adolescents in our community. Physical activity is a vital part of a well-rounded lifestyle. By reducing the rates of growth-plate injuries we are helping to keep the children / adolescents of Dunsborough and surrounding areas active, and lessening the risk of long-term issues related to these growth-plate injuries which can hamper the ability to remain active in the future.
At Dunsborough Physiotherapy Centre we are committed to reducing injury rates in children / adolescents in our community. Physical activity is a vital part of a well-rounded lifestyle. By reducing the rates of growth-plate injuries we are helping to keep the children / adolescents of Dunsborough and surrounding areas active, and lessening the risk of long-term issues related to these growth-plate injuries which can hamper the ability to remain active in the future.
Dunsborough Physiotherapy Centre is a proud sponsor of numerous junior sporting clubs in Dunsborough.
What is a Growth-Plate?
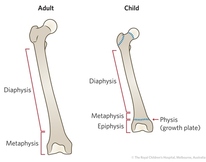 Growth Plate
Growth Plate
The epiphyseal plate (growth-plate) is a hyaline cartilage plate in the metaphysis, at each end of a long bone. This is where bone growth occurs until the growth plate closes (13-15 for girls, and 15-17 for boys).
Growth-Plate Apophysitis / Osteochondrosis: What is it?
 Apophysitis / Osteochondrosis
Apophysitis / Osteochondrosis
At the site of a tendon attaching muscle to bone tractioning (pulling) occurs which stresses the bone. The growth-plate is a weakened point of bone which is susceptible to this tractioning force: swelling and micro-fracture can develop at the site of the growth-plate, hence the painful bump often seen in those sufferers of a growth-plate injury. Growth-plate injuries often occur during growth-spurts (most common in children between 9-15 years old). During a growth-spurt bones grow at a rate faster than muscles can lengthen, leading to increased pulling at the site where the muscle attaches to bone (via a tendon). 20% or more of children will suffer from Osgood Schlatter disease. 2-14% of children presenting with a musculoskeletal injury will have Sever's disease. These conditions create pain and dysfunction (limping, weakness, pain with activity such as running, kicking and jumping, and tenderness to touch at the affected site) for 12 months or more.
3 types of growth-plate injuries addressed by SPRIG program
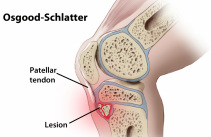 Osgood-Schlatter Disease
Osgood-Schlatter Disease
Osgood Schlatter disease: is a common cause of anterior knee pain in adolescents, affecting the growth-plate of the upper shin bone (tibial tubercle) where the quadriceps tendon attaches. A bump is often seen with Osgood Schlatter disease, and pain is noted when attempting kneeling. Girls who are affected are typically aged 10-11 years, while boys who are affected are typically aged 13-14 years. The condition is more prevalent in active children.
 Sinding-Larsen-Johansson Syndrome
Sinding-Larsen-Johansson Syndrome
Sinding-Larsen-Johansson syndrome: affecting the growth plate at the lower end of the patella (knee-cap): this condition presents similarly to Osgood Schlatter disease: pain with kneeling, running and kicking. This condition is most commonly seen in children aged 10-15 years of age.
 Sever's Disease
Sever's Disease
Sever's disease: affecting the growth-plate of the calcaneum (heel bone) where the achilles tendon attaches: painful during running - children often limit push-off when walking / running. This is often more obvious on the playing field as the player lacks acceleration. The condition is more common in boys than girls (64% boys, 36% girls)
How do I know if my child has a growth-plate injury? The Warning Signs
 Osgood-Schlatter Disease "Bump"
Osgood-Schlatter Disease "Bump"
Tenderness to touch at the growth-plate site: top of the shin where the quads tendon inserts, lower tip of the knee-cap, or at the back section of the heel bone. There may be obvious swelling / thickening at the site.
Pain with activity including running, kicking, and jumping.
Loss of pace, particularly acceleration on the playing field.
Pain with stretching of the quadriceps / calves.
Pain with activity including running, kicking, and jumping.
Loss of pace, particularly acceleration on the playing field.
Pain with stretching of the quadriceps / calves.
Growth-plate injuries: Risk Factors
Inflexibility: during growth-spurts bones lengthen at a rate faster than muscles can accommodate and therefore inflexibility develops. This increases pulling (tractioning) at the growth-plate site.
Poor footwear / poor arch support: footwear with a lack of cushioning / a lack of arch support increases the load through the growth-plates. Greater shock is absorbed through the growth-plate on landing. Over-pronation of the foot also increases load through the growth-plates.
Age (growth-spurts): Osgood Schlatter disease affects boys aged 13-15, and girls aged 11-12. Sinding-Larsen-Johansson syndrome affects 10-15 year olds. Sever's disease affects 10-12 year old boys and girls aged 8-10 years old.
Gender: boys are 2-3 times more likely to suffer a growth-plate injury.
Prior injury: around half the children presenting with a growth-plate injury have had a prior injury to the affected area.
Lack of conditioning: poor muscle tone / endurance and being overweight increases risk of growth-plate injury.
Exercise: active children involved in running, jumping and kicking sports are at greater risk.
Poor footwear / poor arch support: footwear with a lack of cushioning / a lack of arch support increases the load through the growth-plates. Greater shock is absorbed through the growth-plate on landing. Over-pronation of the foot also increases load through the growth-plates.
Age (growth-spurts): Osgood Schlatter disease affects boys aged 13-15, and girls aged 11-12. Sinding-Larsen-Johansson syndrome affects 10-15 year olds. Sever's disease affects 10-12 year old boys and girls aged 8-10 years old.
Gender: boys are 2-3 times more likely to suffer a growth-plate injury.
Prior injury: around half the children presenting with a growth-plate injury have had a prior injury to the affected area.
Lack of conditioning: poor muscle tone / endurance and being overweight increases risk of growth-plate injury.
Exercise: active children involved in running, jumping and kicking sports are at greater risk.
Long-term implications
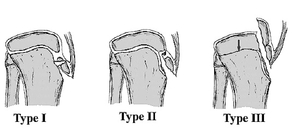 Avulsion fracture: Osgood Schlatter disease
Avulsion fracture: Osgood Schlatter disease
Ongoing pain: pain with kneeling / painful rubbing of the heel in closed-in footwear.
Arthritic change: behind the knee-cap.
Long-term loss of muscle bulk / strength.
Avulsion fracture: a rare complication if not managed correctly
Arthritic change: behind the knee-cap.
Long-term loss of muscle bulk / strength.
Avulsion fracture: a rare complication if not managed correctly
How to Prevent Growth-Plate Injuries
The SPRIG program focusses predominantly on stretching as an injury prevention strategy, though other prevention strategies are documented here.
Stretching: stretching the quads and calves effectively and regularly relieves the pulling force on growth-plates.
Stretching: stretching the quads and calves effectively and regularly relieves the pulling force on growth-plates.
 Orthotics
Orthotics
Good arch support / footwear: to absorb shock, and lessen pronation of the foot - this lessens load through the growth-plate. Orthotics can be useful if footwear does not support the arch of the foot effectively (pictured here). At Dunsborough Physiotherapy Centre we stock a wide range of heat-mouldable podiatry designed orthotics suitable for children.
 Muscle Conditiong Exercises
Muscle Conditiong Exercises
Conditioning: improving muscle strength with resistance work. Most growth-plate injuries occur in the first half of a sports season, possibly due to a lack of conditioning. As muscles fatigue increased load is transferred through the growth-plate. Improved muscular endurance can reduce this load.
 Quadriceps Conditioning Quadriceps Conditioning
Strengthen the quadriceps: try squats, lunges, step-ups, straight leg raise, and VMO exercises.
 Pelvic Stabiliser Strengthening Pelvic Stabiliser Strengthening
Strengthen gluteus medius and minimus muscle groups to improve pelvic stability and lessen deviation at the knee which can lead to overloding of quad / achilles tendons.
|
 Calf Conditioning Calf Conditioning
Strengthen the calves: try heel raises on a flat surface / on the edge of a step. Do these exercises with both straight and bent knees.
 Deep Abdominal Strengthening Deep Abdominal Strengthening
Strengthen deep abdominals to improve the ability of global muscle groups (such as the quads / calves) to function more efficiently - this lessens load on tendon attachments. Check out our Core Strengthening Exercises (Floor-Based / Fitball): click / tap here.
|
Go to our "Physio Exercises" page (click / tape here) for a huge number of exercises including strengthening and stretching exercises for the lower limb.
Contact Dunsborough Physiotherapy Centre
If you have any queries, or think that your child may have a growth-plate injury please call Dunsborough Physiotherapy Centre: phone: 97553600
Proudly powered by Weebly







